What is FEES?
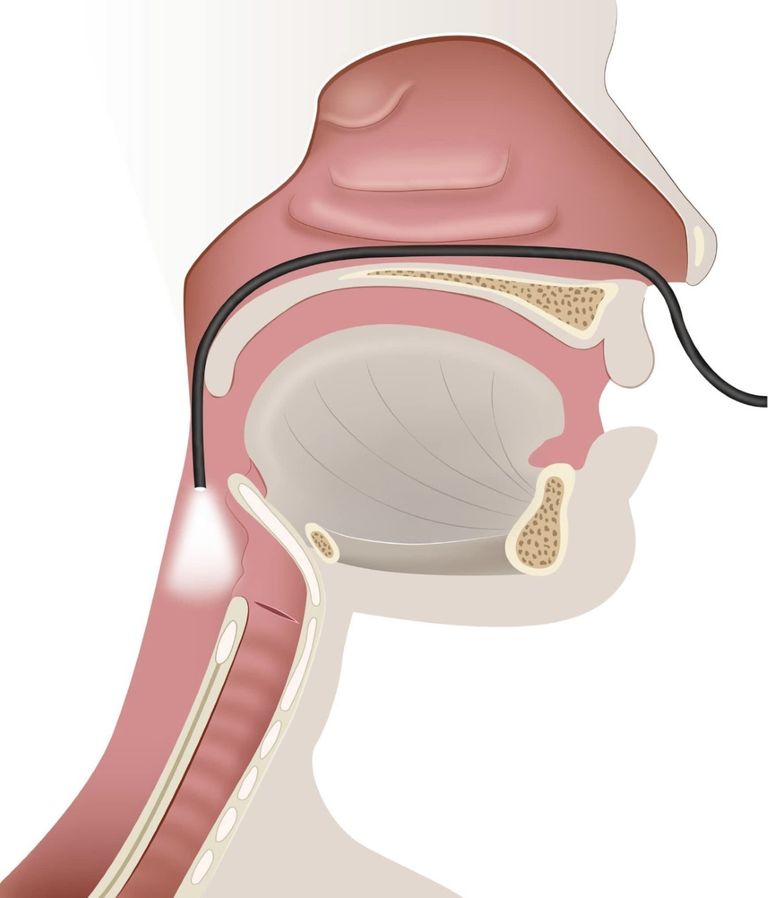
Flexible Endoscopic Evaluation of Swallowing, or FEES, is an instrumental imaging exam used to assess a patient's swallow function. Using a small, flexible endoscope containing a light and camera, a specially skilled Speech-Language Pathologist (SLP) passes the scope transnasally until the pharynx (throat) and larynx (voice box) are in view. The patient consumes a variety of solids and liquids during the exam while the SLP evaluates the anatomy and physiology of the swallow. This includes sensation, presence or absence of aspiration or penetration, effectiveness of the swallow, pharyngeal clearance and use of compensatory swallow strategies. These are areas that cannot be fully assessed or visualized during a bedside swallow exam. Research shows bedside swallow exams have a 70% error rate, where the recommendations are either too restrictive, jeopardizing nutrition and hydration, or silent aspiration is completely missed, which can lead to pneumonia. The exam itself takes approximately 6-20 minutes.
Benefits
• Conducted at bedside.
• Typically done within 1-5 business days after receiving physician's order. Scheduling an outpatient MBSS at a hospital can take several weeks or months.
• Reduces exposure to radiation required for a Modified Barium Swallow Study (MBSS).
• Eliminates need to coordinate transportation to a hospital for a swallow study.
• Reduces need to take staff off the floor to accompany the patient to the hospital.
• Reduces patient fatigue induced by transport to the hospital.
• Reduces hospital re-admissions related to UTI, dehydration, pneumonia, respiratory distress, malnutrition, electrolyte imbalance and more.
• Less expensive than the cost of thickener. $7,000 per year, per patient vs. a few hundred dollars for FEES.
• Less expensive than PEG tube feedings. Estimated cost of 1 year of PEG tube feedings is $31,832.
• Does not affect facility SLP's productivity. SLP can bill dysphagia therapy while assisting with the procedure.
A FEEs can:
- Assess for presence or absence of aspiration or penetration.
- Assess secretion management, laryngeal integrity including tissues and surrounding structures, and any anatomical variations.
- Assess for fatigue or poor endurance for PO intake.
- Assess for specific laryngeal and pharyngeal anatomical and sensory deficits contributing to swallowing difficulty (e.g., vocal cord paralysis, presence/absence of sensation, atypical textures or anomalies).
- Screen for voice changes/dysphonia.
- Assess swallow function pre- and post-op head and neck surgeries, and pre- and post-radiation treatments.
Indications for FEES
Clinical bedside swallow exams are useful in developing a hypothesis regarding the nature of a patient’s swallow function, but they can NOT fully assess the pharyngeal phase of swallowing. An instrumental assessment is the only way to objectively assess the pharyngeal function of the swallow that includes timing, coordination, weakness, and sensation. These are factors that can lead to penetration, aspiration, and residue. Indications that an instrumental exam is indicated would include; patient has a history of dysphagia, is on a modified diet, is feeding tube dependent, is malnourished, has poor PO intake, or patient exhibits swallowing difficulty such as coughing or choking.

